You are dispatched to a lift assist. On scene, you find a male patient who has a gangrenous lower extremity. Upon entering the patient’s residence, you notice squalid living conditions, which indicates that the patient is unable or unwilling to care for himself. It’s your responsibility to convince the patient, who has no mental deficits, that immediate medical treatment is in his best interest, but he doesn’t want to go, despite being the one who called 9-1-1.
As a mandated reporter in your state, does this scenario fit the parameters of neglect or abuse?
Whose duty?
Attorney Sean Flaherty of Ottosen DiNolfo Hasenbalg & Castaldo suggests that first responders can find themselves in more hot water for not reporting than for reporting.
“The easy ones are the easy ones, like elder abuse and child abuse,” Flaherty tells Firehouse Magazine. “The ones where the facts aren’t as clear, the default is, if you can’t make a decision, consult with the other member of your crew, and if it’s a tie, you report.”
Dr. Carlos Falcon, who is the medical director for Des Moines County, IA, explains that, although his county’s EMS providers typically report their findings to the receiving hospital’s nurses and doctors, they aren’t meant to file their own reports with the Department of Human Services.
“Really, it’s a very easy process here,” Falcon says. “The burden is on the emergency department, because we’re stationary. For an EMS crew, even if they’re moderately busy, it’s going to take an hour of their time, and [they] can’t do that,” Falcon says.
Based on suspicion?
Unlike Falcon’s reporting policy, many emergency medical systems across the nation rely on first responders to file the initial report of neglect or abuse.
Paramedic PJ Grouss is a captain with Orange County Emergency Services in North Carolina. He says filing a report starts with his field staff.
“We report it to the receiving physician and the Department of Social Services,” Grouss says. “Law enforcement can get the process going. It’s all about as many statements as you can get.”
Child abuse and elder abuse represent low-frequency, high-risk calls and require mandated reporting. Neglect falls into a gray area. Therefore, EMS providers must know the ins and outs of their state laws.
Still, many providers feel unsure of what steps must be taken and where their obligation ends.
Grouss says that he views this in the same realm as a STEMI (ST-elevation myocardial infarction) activation. “I can recognize one based on my training, but that’s the extent of it, and the main reason is, I’m not a cardiologist.”
So, is it better to activate a STEMI and be wrong? Grouss asks. “Mandated reporting is similar; but also, I don’t want to overreport. You’re asking me to report something that I don’t have hard evidence on and possibly be wrong.”
Nevertheless, Falcon says he would encourage EMS providers to make the initial report, even if it’s based on a suspicion.
“[Doctors and nurses] don’t go to the house, and [they] don’t see the living conditions,” Falcon says.
Almost as a supplement to mandated reporting, Grouss says in Orange County a community paramedic program was implemented to flag high-risk individuals in their patient-care reporting software. Although more of a “fall-risk” program, its members can identify other potential problems.
Grouss explains that, each morning, the program receives a list of patients who require follow-up. “They’ll go out and do an assessment and work with Department of Aging,” which will look at trip hazards or install handrails. “If we get to a point where the patient is declining [assistance], we look for an alternative with [the Department of Social Services],” Grouss says.
The bottom line
Without clear and defined mandated reporting procedures, EMS providers might believe that their efforts often fall on deaf ears.
“I’ve done reporting and a brief interview, and it fizzled out, and you don’t know what came of it,” Grouss says.
Falcon suggests that some means by which EMS could know the outcome of their report would be beneficial. “If we never see any outcome, it’s not encouraging [to the crews] to continue to make reports.”
Even when abuse and/or neglect is just a suspicion, Flaherty, Grouss and Falcon agree: The appropriate course of action is to report your findings.
“It’s very helpful,” Falcon says. “A lot of cases get looked into even if no charges are ever pressed.”
About the Author

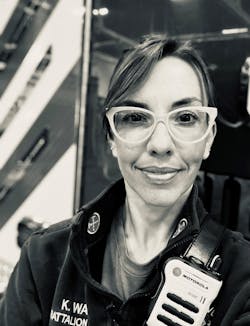
Kristen Wade
Kristen Wade is a battalion chief and EMS program manager with the Sugar Grove, IL, Fire Protection District and is in charge of an engine and ambulance company. She has nearly two decades of experience in the fire service and 15 years of experience as an Illinois licensed paramedic. Wade served as an instructor for the Illinois Fire Service Institute’s fire officer program. She is certified by Illinois Firefighter Peer Support. The organization focuses on the mental health and wellness of EMS and fire personnel. She obtained a bachelor’s degree in English communications from Fort Lewis College.