Every fire department knows that lift assists are a normal part of the job. In fact, it probably is safe to assume that a department’s most numerous type of call is from a person who needs assistance to move out of a chair or bed or who fell but doesn’t need emergency care. Not only is the volume high, but it also is very likely that lift-assist callers dial the station often, perhaps even multiple times on the same day. Recent data from a Midwestern fire department indicate that slightly more than 10 percent of its total calls were related to lift assists.
With the high volume of calls and the repetitive nature of lift-assisting, it can be easy to fall into complacency in terms of care. It might be tempting to go through the motions and not stop to consider the whole person and that individual’s environment. For example: How does the person respond to you? If the person called previously, does the individual seem different than the last time? How often does the person call, and is it for the same reason or does it vary every time? Are there any risk factors in the person’s physical space? Do people check in on the individual?
This is where a shift in focus can transform the outcomes of these patients and also the fire departments who care for them. There is a significant, yet simple, opportunity to change how departments think about and treat these callers so that everyone benefits, particularly those who call on members for help.
The shift is toward prevention, and it can begin through some basic steps that any department can implement right away.
Mine your call data
How many of your department’s calls are lift assists? Are your top 10 callers to the department lift-assistance-related?
Having these data points can benefit departments in a couple of key ways.
First, it provides a real situational baseline to understand the needs that are in the community and the magnitude of effect that a new approach that’s focused on prevention can make. Decreasing the number of lift-assist calls can allow departments to spend more time and energy on preventive care/programs. There can be more time for the acute emergency calls that the department answers on any given day, too. How much time and effort that would be saved is based on the call data?
Second, understanding the data gives a department greater insight into the people who are most vulnerable to and at risk of falling and other medical issues. By reviewing the frequency of lift assists by patient and then ranking across all callers, departments can begin to see patterns that point to potential catastrophes down the road. Preventive measures can be prioritized for those who are at most risk and can help departments themselves in the end to reduce overall lift-assist volume by tackling the most predominant cases first.
As with most things in life, data are your friend. They can help assess, prioritize, and target meaningful change throughout the department and community.
See the whole person
The people who are on the receiving end of care need more attention. Because lift assists can be so routine, departments might be unconsciously blind to patterns that are within this population, such as an aging woman who fell three times in the past week while her vitals decline. Members might miss the fact that an elderly man who lives alone keeps tripping on the same rugs and low furniture.
To increase visibility, departments can put some simple practices into place very quickly that will help them to see the whole situation that’s in front of them.One idea: Get vitals on each lift-assist patient and then document the vitals in whatever medical software that’s used within the emergency care system. Not taking vitals is a lost opportunity to gather data and assess the person as a whole.
Another idea: Ask more questions. How does the patient feel? When was the last time that someone checked on that person? Does the person need help with meals, hygiene or cleaning chores around the home? How recently has the individual had a visit with a primary care physician?
By asking and then listening attentively, so much can be learned about the patient’s true needs, and once true needs are known, preventive and supportive care can follow in a meaningful way.
Document more
Creating a documented history on lift-assist patients is yet another simple recommendation for improvement. As mentioned above, when vitals are taken, document them for future reference in a system that’s accessible across the department and, possibly, the broader medical team. That way, information is readily available when patients call again, and insightful patterns might emerge.
Records do matter. Historical documentation and ongoing analysis can help to identify at-risk individuals who need preventive care the most.
A ground-breaking program in the greater Columbus area of Ohio has proven the positive effect that a multidisciplinary, preventive approach to lift assists can have on a department and the community that it serves.
Leading the way
Through a partnership between the Upper Arlington, OH, Fire Department and The Ohio State University Wexner Medical Center, an innovative pilot program was designed and implemented into the local community. At its core is the fundamental belief that treating and, ultimately, preventing falls require an integrated, multidisciplinary approach to these patients.
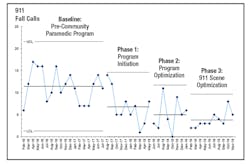
The Community-centered Fall Intervention Team model, or Community-FIT for short, launched in 2016.Through Community-FIT, several practices were put into place that continue to make a huge difference. One of them is a Patient Acuity Scoring framework that has helped fire departments to categorize patients on their fall risk. With this information, the appropriate preventive follow-ups and services can occur.
Another was the activation of supplemental assessment activities, services and support teams to further promote prevention. For example, as part of the home visit screen, a patient’s mental health is assessed in addition to the individual’s physical vital signs. Findings and recommendations of the home visit screen then are delivered to other healthcare professionals, and the patient is connected to local resources and programs as needed.
Real effect
The results of the Community-FIT program are astounding. Fall calls in the community declined by 66.7 percent over a three-year period. Fall calls that resulted in transport to an emergency facility declined by 64.2 percent, which supports the belief that a shift in focus to prevention is transformative.
To sum it all up, a Community-FIT team member states, “There are many gaps in healthcare that can be addressed with teamwork and thinking about the critical points of action for teams to tackle hard problems. What gap can you fill? If it is lift assists, there is a growing number of models to work from and evidence that they can make an impact.”
So, as you consider your approach with lift assists, remember that fire departments can start with some quick and basic steps on the road to fall prevention. By looking at the data, paying attention to the whole person and the individual’s surroundings, and documenting what you learn, your department can be well on its way to changing outcomes for the better. Sometimes, all it takes to begin is a shift in focus.
About the Author
Mindy Gabriel
Mindy Gabriel is the deputy fire chief in charge of EMS operations for the Westerville, OH, Fire Division. She oversees EMS emergency operations, tactical EMS, outreach education, training, quality improvement and a community paramedic pilot program. Gabriel serves as the department's infectious control officer. Previously, she served 17 years with the Upper Arlington, OH, Fire Division. Gabriel’s background in community EMS services and working with fellow firefighters as a peer counselor includes developing innovative programs for a changing fire-based EMS service. She has a bachelor’s degree in education from The Ohio State University.