As emergency responders, we are tasked with executing lifesaving maneuvers in high-stress situations. For example, every one of us has been trained to know the traditional ABC sequence of trauma care—airway, breathing and circulation—or, as we now know, CAB, with circulation before airway.
We also know that time equals brain cells. We can’t allow patients to go without lifesaving oxygenated blood for an extended amount of time.
The airway and the tools that we carry in our quiver changed over the years, and a quick and hassle-free device replaced, for all intents and purposes, the need for traditional intubation in a high percentage of patients.
I’m referring to the i-gel and i-gel O2 Resus (short for resuscitation) Pack by Intersurgical out of the U.K.
For those readers who are unfamiliar with the i-gel and i-gel O2 Resus pack, I’ll break it down for you.
i-gel and i-gel O2
Intersurgical claims that the i-gel is ideal for emergency medicine and difficult airway management, because it provides high seal pressure and reduced trauma and incorporates a gastric channel to protect against aspiration.
The i-gel O2 includes a small supplemental O2 port, so first responders can supply passive oxygenation as a component of CPR.
Think of it this way: The i-gel is like a supraglottic bag-valve mask (BVM). The device creates a seal directly over the pharyngeal, laryngeal and perilaryngeal structures. There’s no balloon to inflate, and insertion is very straight forward, literally. Providers no longer must insert and twist the device, such as is required of laryngeal tubes.
However, as with laryngeal tubes, providers can perform a blind insertion and rest assured that the device is properly placed.
Also of note, the i-gel and i-gel O2 both contain a gastric channel, which allows providers the ability to suction regurgitant or stomach contents. The i-gel and i-gel O2 both have a standard 15 mm connection for ease of use with a BVM.
Cody Brumm, who is a paramedic in northern Illinois who has 15 years of street experience and has instructed future paramedics for 10 years, says of the i-gel, “It allows us to place it in with minimal fail.”
Specific to the i-gel and i-gel O2, the devices contain an integral bite block and boast three adult sizes. The i-gel comes in two pediatric sizes, one infant size and one neonate size. All sizes are contained in color-coded packaging.
It was evident after speaking with Brumm that many EMS systems across the country are catching on to what began as a tool that was used primarily in anesthesia and surgical rooms.
“I’ve seen more EMS systems moving toward supraglottic airways as their airway of choice,” Brumm says. “Some systems show preference to that.”
Specifically in the event of a cardiac arrest, Brumm explains, “The use of the i-gel allows us to place an advanced airway without interrupting chest compressions, and there is less of a chance of complications.”
Don’t ignore intubation
Among its many advantages, the i-gel also was a go-to airway device at the height of the COVID-19 pandemic.
I work in an EMS system that mandated a stop during the pandemic to all aerosolizing procedures, such as endotracheal intubation. Such procedures had the potential to rapidly spread the virus from patient to provider or patient to emergency room staff. Therefore, when a secure airway was required, the i-gel was used with great success.
However, Brumm warns that with the increased use of the supraglottic airway devices, there’s the risk of dulling the skills that are necessary to perform an intubation using a traditional endotracheal device. He recalls a time not too long ago when the practice of performing a traditional intubation nearly was removed from paramedic curriculum because of a low success rate.
That said, intubation combined with capnography provides paramedics with the tools that are necessary to be proficient while performing an invasive procedure.
Brumm compares the lack of practiced skills for a traditional intubation with the feeling that some of his paramedic students expressed when caring for a neonate or a pediatric patient.
“If you’re feeling uncomfortable in those skills, you’re less likely to go to them. So, in adult intubation, if we don’t keep practicing those skills, there is a likelihood of becoming unfamiliar in it,” Brumm says.
The moral of the story is, although the use of the i-gel or i-gel O2 is efficient and highly successful, don’t get rid of your endotracheal tubes just yet.
In situations where an i-gel is contraindicated, such as anaphylaxis and patients who have sustained thermal injury to their airway, paramedics must be able to effectively deliver lifesaving interventions, such as endotracheal intubation.

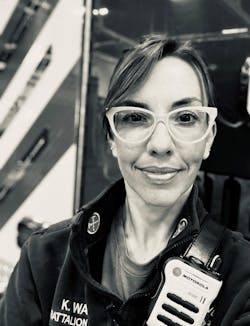
Kristen Wade
Kristen Wade is a battalion chief and EMS program manager with the Sugar Grove, IL, Fire Protection District and is in charge of an engine and ambulance company. She has nearly two decades of experience in the fire service and 15 years of experience as an Illinois licensed paramedic. Wade served as an instructor for the Illinois Fire Service Institute’s fire officer program. She is certified by Illinois Firefighter Peer Support. The organization focuses on the mental health and wellness of EMS and fire personnel. She obtained a bachelor’s degree in English communications from Fort Lewis College.